To Screen or not to Screen?
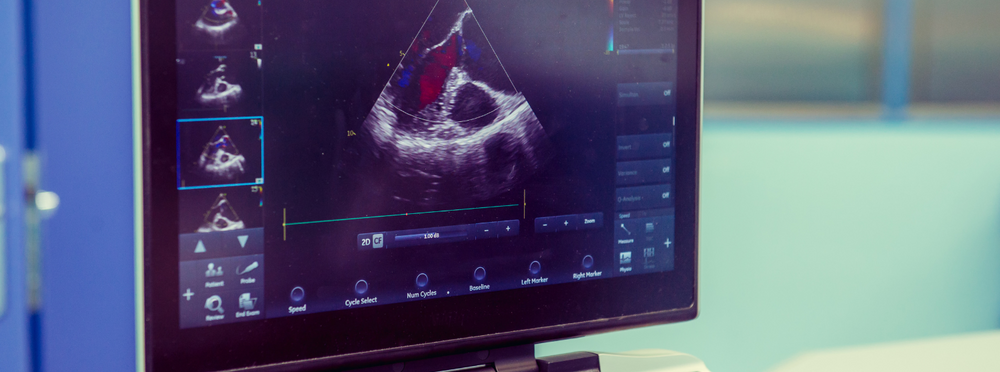
Medical technology is always advancing. We can look at your neck, abdominal and leg arteries and screen for blockages and aneurysms. We can measure the thickness of the lining inside your arteries and determine your “vascular age”. We can look for calcium in your heart arteries to detect plaque build-up way before a stress test would. And you don’t even need a doctor’s referral to get screened. Sounds pretty exciting.
Many companies offer heart and vascular screening. I provide this type of screening in my office. But just because a test is available doesn’t mean you should have it done. You should only have a test if it will affect your care.
In reality, many people don’t need these tests. If you’ve already had a heart attack or bypass surgery or a stent, you have diabetes, or everyone in your family developed heart disease in their 50s, there is no amount of screening that will dissuade any care giver from advising you to be maximally aggressive in terms of your prevention efforts. In other words, the test results – regardless of what they are – will not affect your care.
But what if the situation is less clear? Maybe you have elevated cholesterol readings but everyone in your family had that too and lived into their 90s. Do you need to be on a statin drug? Or all your numbers are perfect, but your mom just had a heart attack, and there had been no clues that she was at risk.
When it’s not clear how aggressive to be in terms of risk factor control – and especially deciding whether you need additional medications – taking an extra step to get more objective data about the status of your arteries can make a lot of sense.
8 points to remember:
- Vascular screening tests are progressively less helpful with increasing age. Almost all of us will develop some atherosclerosis as we get older so the discriminating value falls off, especially over age 65 for men and over age 70 for women. There is one exception for male smokers. One time screening for abdominal aneurysm is advocated (and covered by Medicare) for this group between age 65 and 75.
- If the test is “positive”, don’t panic. The abnormalities detected almost certainly did not happen overnight. You are fundamentally no different than you were 6 months ago or even a year ago. We just happen to have more information about you now – and can adjust your treatment based on new facts.
- Once abnormal, there is no reason to repeat any vascular screening test. You have already learned everything you can learn from the test.
- If the test is “negative”, it does not give you permission to abandon heart healthy habits or start smoking. The test is only one data point and has to be viewed in the context of your overall health and risk factors.
- Beware of “incidental” findings. Sometimes a screening test can incidentally pick up an abnormal finding outside of the cardiovascular system. Most of these findings end up being benign, but will require follow up. There is some truth to the adage that tests beget tests. This is one of the reasons why screening should not be undertaken lightly – sometimes the downstream risks associated with following up every abnormality detected are higher than the risks of having the original problem you were trying to evaluate.
- No test is a substitute for common sense. If you are experiencing squeezing chest pain every time you walk up a flight of steps and a screening test is normal, it could still be your heart. You should never ignore any symptoms or attempt to self-diagnose.
- If you are getting this done because you are feeling frustrated that your doctor is not listening to your concerns, the answer might be to find a different doctor, rather than getting a screening test. You’re going to need a health advocate regardless of the test results.
- No matter how the test turns out, your best defense against developing heart disease – or requiring medications to control risk factors – is to eat a diet rich in whole food fiber, omega 3 fatty acids, antioxidants and plant sterols. In fact, improving lifestyle, and especially food intake, is more impactful in affecting health outcomes than any drug, test or procedure.

Tested & Proven Results.
- Cardiologist formulated
- Supported by over 500 publications
- Clinically-proven, in a double-blind randomized trial with Mayo Clinic and The University of Manitoba
80% of participants lowered their cholesterol in just 30 days. With just two servings per day, Step One Foods offers a proven-effective way to naturally lower LDL (bad) cholesterol.
Get heart health tips and articles like this, delivered right to your email.
New articles every week.
You may also like...

Spring Into Heart Health: The Best Seasonal Foods to Eat Now

You don’t need to avoid foods with cholesterol…except for these



